Dementia cure sought in living brain tissue cells

* The article you are about to read is a news article compiled from The Guardian's Health News.
In a breakthrough that could accelerate the search for a cure, scientists have used living human brain tissue to mimic the early stages of Alzheimer's disease, the most common type of dementia.
In this world-first study, conducted by a British team, they showed how exposing healthy brain tissue from cancer volunteers to a toxic form of a protein linked to Alzheimer's - taken from patients who had died from the disease - disrupted the connections between brain cells in real time.
The groundbreaking move has offered a rare and powerful opportunity to see how dementia develops in human brain cells . Experts say the new way of studying the disease could make it easier to test new drugs and increase the chances of finding ones that work.
Dementia poses a major threat to health and social care systems worldwide. As we approach a future that could overwhelm many countries in terms of both human resources and needs, as many neurological conditions require long-term care, the projected figures prove this thesis. The number of people affected by dementia and related diseases is projected to triple today to approximately 153 million by 2050. This highlights why finding new ways to study the disease and accelerate the search for a cure is a health priority.
In the study, scientists and neurosurgeons in Edinburgh have teamed up to show for the first time how amyloid beta , a toxic form of a protein linked to Alzheimer's, can attach to vital connections between brain cells and destroy them.
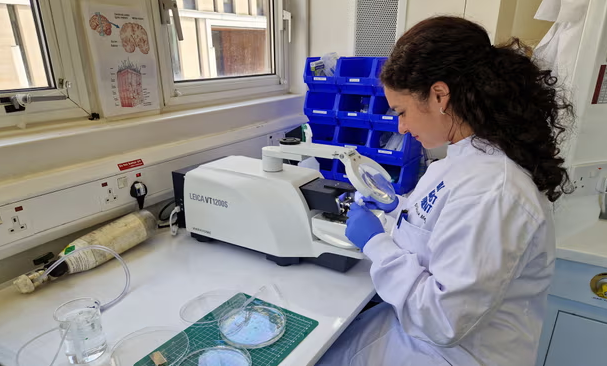
Small pieces of healthy brain tissue were collected from cancer patients undergoing routine surgery to remove tumours at Edinburgh Royal Infirmary.
Once the brain particles were removed, the scientists placed the samples in glass vials filled with oxygenated spinal fluid before boarding taxis to transport them to their labs a few minutes away.
" We immediately ran back to the lab ," said Dr Claire Durrant, a Race Against Dementia fellow at the Centre for Discovery Brain Sciences at the University of Edinburgh and the new leader of the UK Dementia Research Institute.
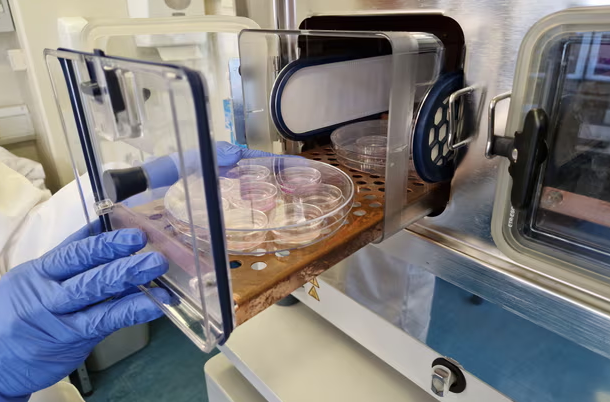
There, the samples were cut into pieces less than a third of a millimeter thick and placed in small dishes. Each piece of living brain tissue was kept in a nutrient-rich liquid inside a 37-degree Celsius incubator to mimic body temperature. “And then we pretty much started experimenting,” Durrant said. The pieces of human brain were kept alive in dishes for two weeks, with the patient’s permission.
The researchers extracted the toxic form of amyloid beta from people who had died of Alzheimer's disease and then applied it to healthy living brain tissue in dishes. "We're trying to mimic Alzheimer's disease," Durrant said.
His team found that the brain did not try to repair the damage caused by the toxic form of amyloid beta as it does when exposed to a normal form of the protein .
Even small changes in natural levels of amyloid beta—up or down—were enough to damage brain cells. Durrant said this suggests that the brain needs precisely tuned levels of the protein to function properly:
- Working with the neurosurgical team at the University of Edinburgh, we have shown that living human brain tissue can be used to investigate fundamental questions about Alzheimer's disease. We believe the experiments could help transfer findings from the lab to patients more quickly, bringing us one step closer to a world free from the heartbreak of dementia.
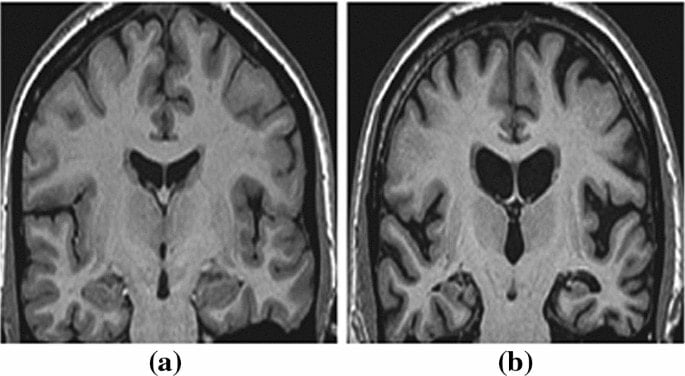
The breakthrough will allow scientists to focus on drugs that have the best chance of preventing the loss of synapses, the connections that allow messages to flow between brain cells and are vital for healthy brain function. Alzheimer’s attacks synapses , and their loss strongly predicts poor memory and thinking ability .
Durrant's team also found that brain slices taken from the temporal lobe, an area known to be affected in the early stages of Alzheimer's, produced higher levels of signal.
TAU PROTEINThis result may explain why this part of the brain is particularly vulnerable in early Alzheimer's, as increased release of tau protein may allow toxic forms of this protein to spread more quickly between cells.
The research was supported by a £1m donation from Race Against Dementia, a charity set up by Sir Jackie Stewart after his wife's dementia diagnosis, and the James Dyson Foundation, a charity supporting medical research and engineering education.
Dyson said the breakthrough represented progress "towards solving one of the most disruptive problems of our time":
- Collecting samples of living human brains and keeping them alive in the lab, along with neurosurgeons and their volunteer patients, is a groundbreaking method that has allowed researchers to better study Alzheimer's disease in real human brain cells rather than relying on animal substitutes such as mice.
Professor Tara Spiers-Jones, group leader at the UK Dementia Research Institute, explained the significant development:
- The study provides a new tool for scientists to see early Alzheimer's in real time, better understanding the disease and how to treat it. The use of living human tissue samples generously donated by people who have had surgery to remove brain tumors allows scientists to study how the living human brain responds to the toxic proteins produced in Alzheimer's, and in the future, will allow new treatments to be tested in human brains to see if they are effective.
*** The Guardian
*** Health Editor - Andrew Gregory
SÖZCÜ