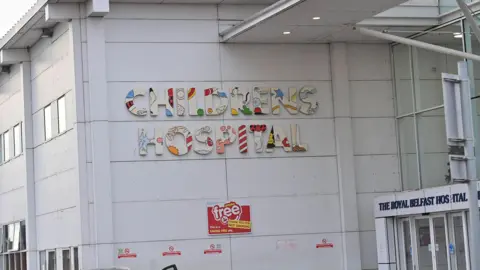
'Broken and burnt out': Nurse lifts lid on staffing at children's cancer unit

A whistleblower who resigned from the Royal Belfast Hospital for Sick Children over staff shortages has said the system left her broken, disillusioned and burnt out.
Hannah Farrell, who left the Children's Cancer Unit in 2019, said the lack of support and management's failure to listen to her and other nurses led her to resign.
Parents of sick children and former staff members contacted BBC News NI after it was revealed more than half of the specialist nurse team at the cancer unit are currently off work, a problem that Ms Farrell said was not new.
In a statement, the Belfast Health Trust said there had been "significant investment" in the unit's service development in the last decade.
It added that this included "an increase across all nursing bands, and the development of specialist nursing roles".
The trust said it wanted to thank the "hard-working nurses" and wider staff at the unit for their work "particularly during times of pressure, to ensure the safe and timely care of our patients and the support they provide to families".
Ms Farrell said that for years maternity leave, long-term sickness and career breaks at the unit were not backfilled, meaning wards were insufficiently staffed.
She said that raised pressure on colleagues and had the potential to impact patients, but the issues were not addressed.
"When a ward goes into crisis like it did a few weeks ago, the trust takes nurses from other wards, which just puts a band aid on it," she said.
"It's a quick fix, all we've done is impact other wards negatively and we haven't fixed the problem."
During her five years as a nurse at the unit, treating some of Northern Ireland's sickest children, Ms Farrell often had to deal with the pain of a patient's death - however, she was not offered counselling and had to pay for it herself.
Belfast Health Trust said it has a specialist occupational health that offers "individualised support to staff" and that staff can also "avail of a number of services that offer physical and psychological support".
"We encourage staff to raise concerns within their teams and with line managers," it added.
Ms Farrell, who still works as a nurse in the health service, said she was speaking out in the hope it will help nurses who feel their voices are "silenced" by management.
"The system took my fight, my joy, my empathy and compassion - I had nothing left to give.
"I dreaded every shift because I didn't know what I was going into, staffing-wise, or what the skill mix would be.
"Clearly nothing has changed since I handed in my resignation five years ago, so nurses have no choice but to go off sick."

The Children's Cancer Unit is the regional centre where children in Northern Ireland are treated for cancer or a complex blood disorder diagnosis.
Specialist cancer nurses are specially trained to administer treatments including chemotherapy.
Seven out of 12 specialist nurses are currently not working, which meant some treatment was postponed earlier in August.
According to the trust about five children were affected and have since received their treatment.
However, parents of patients treated in the haematology and oncology wards in years past told BBC News NI they saw nurses regularly under pressure due to staffing problems.
David and Sara Watson's son Adam underwent treatment for acute myeloid leukaemia at the Children's Cancer Unit between 2019 and 2022.
Adam, who died in 2022, was nine when he helped set up the B Positive charity to support families and specifically to provide counselling to nurses on the ward.
David Watson said the clinical service is world class but often the wards are understaffed, and nurses regularly stay on after their shift.
"This isn't a new problem - staff are being let down by the Belfast Trust, by the Department of Health and, ultimately, by the health minister.
"He's the boss at the end of the day.
"People need to sit down and study the statistics - why are nurses off sick and why are they leaving?"
A statement from the Department of Health said the minister fully acknowledges the staffing challenges facing the Belfast Trust and wider system.
"He recognises the efforts made by Belfast Trust to manage and address the recent nurse staffing issues within paediatric haematology and oncology, and notes assurances given by the trust that service delivery is being closely monitored."

Sara Watson said it was "no way to run a hospital" and that any other business would forward plan, especially around maternity leave cover.
"The powers that be don't seem to understand the skills required for this ward to function."
Caroline and Martin Smyth, whose son Theo was treated at the cancer unit in 2020, told BBC News NI they also witnessed first-hand how staff shortages affected the haematology and oncology wards.
"The nurses are run off their feet and they are dealing with some of the sickest children in Northern Ireland.
"The 10-bed ward was always full - yet there wasn't always a full quota of staff, especially at the weekends."
The Belfast Trust told BBC News NI there are currently "no nursing registrant vacancies" at the Children's Haematology Unit.
It added that all nursing roles in the haematology and oncology departments had been reviewed "which enables the trust to utilise staff from the wider team in other ward areas and bank staff to safely cover the service when required and protect the most time critical treatments".

Ms Farrell, who keeps in touch with staff still working there, said the unit is operating on the "fumes" of the nurses' good nature.
She said her last three overnight shifts on the ward were "horrendous" as too much responsibility was placed on her shoulders.
"I oversaw a full ward of seriously-ill children, some were dying, and I was supported by a bank and a junior nurse - it just broke me."
She said the children and families "deserved the highest and best level of care" but that she did not feel she "had the ability or the support" to deliver it.
Ms Farrell said the NHS promoted an 'it's OK to not be OK' attitude around mental health, but expected its nurses to give more than they can.
She said she can still recall the names and faces of the 56 children who died in her care but said at no time was she offered counselling.
"You're expected to just pick yourself up and go into the next room - the impact is massive."
BBC





