Surgery for depression is a milestone in Colombia: 'It's a last resort' and is covered by the EPS.

Lorena Rodríguez is 38 years old and has been battling depression for over two decades, a condition that even six different treatments have failed to address. During this time, Rodríguez has threatened her life, experiencing days when she was unable to get out of bed, work, or interact with anyone. All that changed a few days ago when a team of doctors and neurosurgeons implanted several electrodes in her brain, a surgical milestone for the country.
The innovative procedure, called Deep Brain Stimulation (DBS), was performed at the International Hospital of Colombia (HIC) and involved the implantation of four electrodes in different deep regions of the brain. These electrodes were connected to a battery in the chest, which emitted continuous electrical impulses to regulate brain activity, adjustable by remote control.

The entire procedure was performed while the patient was awake and monitored. Photo: HIC
“In this case, four perforations were made in the skull. Until now, only two were normally made, because only two electrodes were implanted, but in this procedure, we placed four—which, in technical terms, is actually six. Four small holes were made, approximately 4 millimeters each, and the surgery was performed with the patient lying down and awake. Before implanting the final electrode, a catheter is inserted that acts like a lightning rod and records the electrical activity of the neurons in the specific area to be reached,” explains Dr. William Omar Contreras, functional neurosurgeon and HIC research associate.
The procedure involved precise planning using advanced brain imaging techniques such as tractography, which allows for mapping emotional circuits. “This is like sending a missile to a specific location,” the specialist notes. The surgery is performed with the patient awake to monitor the immediate effects of brain stimulation. “She was smiling intraoperatively. It was a beautiful result,” the doctor adds.
Ultimately, the entire system remains inside the patient's body, and the patient will live with the electrodes for the rest of their life and continue to be monitored medically. From time to time, Lorena will have to undergo surgery to replace the electrode batteries, which remain attached to the patient's chest. "The patient can go to the sea, fly, or go about their normal life. Nothing is exposed," explains Contreras.

The entire procedure was performed while the patient was awake and monitored. Photo: HIC
The procedure isn't a definitive cure, but it does offer a functional alternative for patients whose quality of life is severely limited. "We don't cure anything, but we do improve the patient's quality of life. She can go out again, work, socialize, and feel interested in a partner," explains the specialist. Lorena had tried six types of antidepressants, cognitive-behavioral therapies, transcranial magnetic stimulation, and other treatments without lasting results. "She was someone who was almost certain to commit suicide. She had already attempted suicide. We went through a two-year process to determine whether we could effectively perform the intervention," adds Contreras.
The expert emphasizes that this type of surgery is only considered in extreme cases, after all conventional alternatives have been exhausted. “Patients must be evaluated by at least two independent psychiatrists. Both must agree that all possible alternatives have been attempted,” Contreras explains. In addition, other interventions such as electroconvulsive therapy or repetitive transcranial stimulation must have been performed. Because surgery is minimally invasive and has a continuous effect, it represents a hopeful option for those who have lived with disabling depression for decades.

The operation required a multidisciplinary team of experts led by Dr. Contreras. Photo: HIC
More than 400 surgeries similar to this one have already been performed worldwide—the first in Canada. But the one performed at HIC is different due to its complexity and multiple approaches. “Until now, the usual approach was to implant only two electrodes. We implanted four, with stimulation directed at six different structures. It's a pioneering surgery,” Contreras points out. The approach seeks to modulate not only profound sadness but also associated symptoms such as anxiety, guilt, and mental rumination. “Emotional circuits don't only pass through Highway 25 in the brain. Other 'avenues' must also be stimulated to obtain more comprehensive results,” he adds.
This breakthrough is the result of Contreras and his team's prior experience in complex procedures such as surgery for severe aggression, patients with autism spectrum disorders, and diseases like Parkinson's. "I have worked in different parts of the world and have led research on cerebral microdialysis. All of this has allowed this surgery to take a different approach," says the neurosurgeon. The operation symbolizes not only a technical evolution, but also a paradigm shift in the treatment of serious psychiatric illnesses through functional neurosurgery.
It's important to highlight that the milestone achieved is also a reflection of collaborative work across multiple disciplines. This was an effort by a functional group comprised of neurologists, psychiatrists, neuropsychologists, epidemiologists, and electrophysiologists, including, for example, Dr. Paula Millán and Dr. Juan Esteban Rosales. This integration has been key to planning and individualizing the intervention, from patient selection to postoperative follow-up.
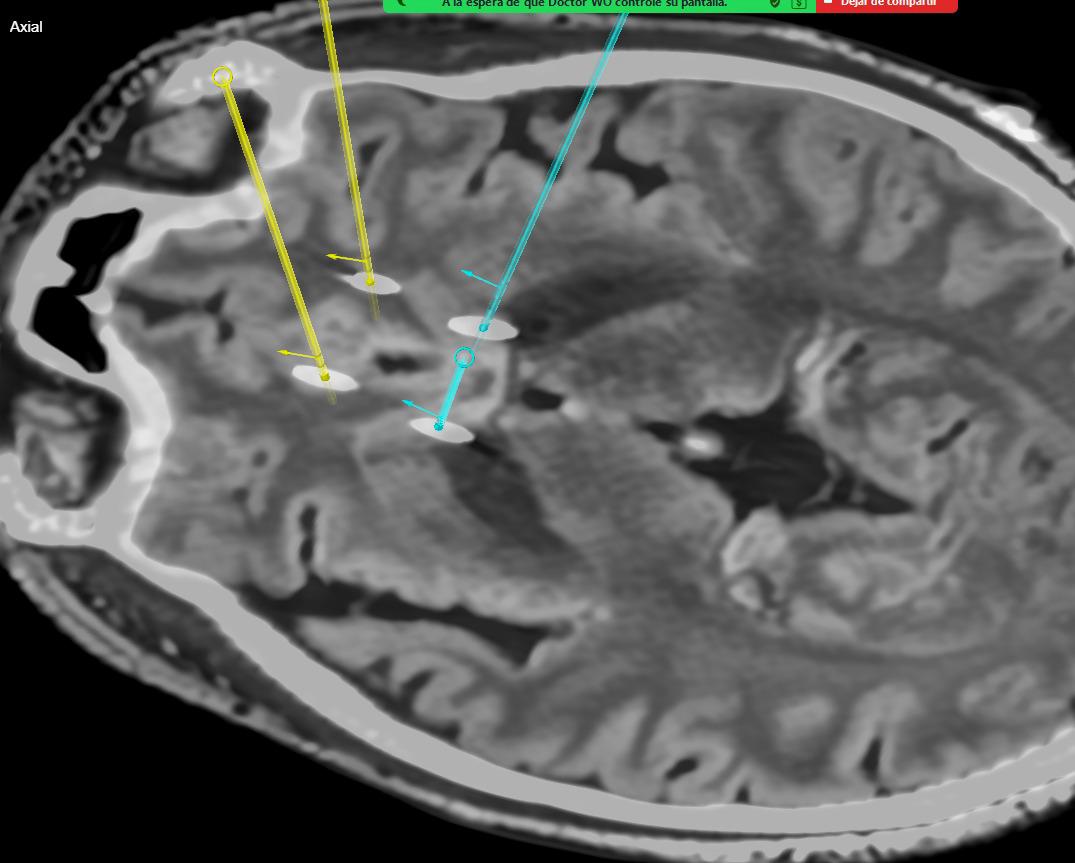
The electrode system will remain implanted in the patient for life. Photo: HIC
And, despite its complexity, the surgery is covered by the Colombian healthcare system. “Patients have the right to surgery through their EPS (Health Insurance Company), as long as they meet the clinical requirements and pass through the medical committee. The problem is that many don't know it exists, and sometimes even the treating physicians don't refer them,” explains Contreras. The specialist's call is to educate and destigmatize: “This isn't a lack of character. It's an internal storm that often can't be faced alone. There is hope, there is science behind it, and there is access,” he concludes.
Depression: A global disease that demands attention According to the World Health Organization (WHO), depression affects 5 percent of the global adult population, with approximately 280 million people suffering from this condition, a number that is increasing. Of these, 70 million are refractory cases, meaning they do not adhere to or show improvement with any treatment, and an estimated 350,000 could be candidates for DBS worldwide.
Deep brain stimulation for depression is still a rare procedure, but with promising results, according to Contreras. A long way from a study in which we can clearly assess its impact on patients in comparable numbers is still a long way off. However, it is an available alternative for extreme cases that also sets Colombia as a global example in neuromodulation and interventions of this type.
In that sense, Lorena, the patient who underwent surgery, appealed to those struggling with mental illness: “The life we have will always be worth living. Let's not underestimate ourselves, let's not think we're weak. We have to talk, we have to seek help. We should all have a primary care psychologist. Mental health is debilitating, sometimes more so than a physical illness.”
Environment and Health Journalist
eltiempo

%3Aformat(jpg)%3Aquality(99)%3Awatermark(f.elconfidencial.com%2Ffile%2Fbae%2Feea%2Ffde%2Fbaeeeafde1b3229287b0c008f7602058.png%2C0%2C275%2C1)%2Ff.elconfidencial.com%2Foriginal%2F624%2Fbb6%2F395%2F624bb6395f63c9c60981b5a9c1328633.jpg&w=1280&q=100)



